Case guesses:
Mike writes:
Hi guys
I was first considering giardia but Daniel mentioned it in his description so I am now leaning toward Tropical Sprue causing the flattening of intestinal villi, steatorrhea and malnutrition. Cause unknown?
Happy sailing,
Mike in Oregon
Wink writes:
If Dixon was advised to look this one up, I certainly had to. I came up with capillariasis. C. philippinensis is not uncommon in the Philippines and Thailand. Humans acquire the parasite through ingestion of raw freshwater fish (as with Koi Pla). Adult C. philippinensis worms in humans can release eggs that hatch into larvae in the intestine and cause hyperinfection and possibly voluminous stools and wasting. Albendazole can be curative.
Wink Weinberg
David writes:
Dear Esteemed Doctors,
I did not write in last week, but I did guess correctly that the patient had contracted Naegleria fowleri – my condolences to the family.
As for the case of the Thai fisherman struck with bouts of diarrhea, I believe this man has contracted a case of opisthorchiasis caused by the Southeast Asian liver fluke Opisthorchis viverrini. A quick Google search and some research led me to sources that connected many Thai and Laotian dishes featuring raw fish (koi pla, pla ra, and som tam) with liver fluke disease.
This disease is contracted by humans consuming raw fish infected with the metacercariae of the fluke. The metacercariae excyst in the duodenum, and ascend through the ampulla of Vater into the biliary ducts of the liver, where the parasites attach and mature. The adults lay eggs after 3-4 weeks, which are passed in the feces and consumed by the primary intermediate host – a snail. Miracidia hatch in the snail, and eventually develop into cercariae, which leave the snail and seek freshwater fish (the secondary intermediate host). In the muscles or under the scales of the fish, the cercariae encyst into their metacercariae stage, which are then consumed with their fishy hosts by definitive host mammals (cats, dogs, humans) and thus the life cycle is complete.
Diagnosis should be confirmed by examining the stool for eggs or performing an ELISA on an 89 kDa antigen of the parasite, and treatment includes the antihelminthic praziquantel.
The first week of graduate school has been fair, but I am chomping at the bit to get in the lab and start tinkering with those schistosomes.
Best wishes,
David P.
To answer the question to the lyric, “So come up to the lab and see what’s on the slab”, this line was immortalized by the great Tim Curry in the cult movie musical Rocky Horror Picture Show, written by Richard O’Brien.
Steve writes:
Salutations TWIPtoids!
Our case of the Thai fisherman with chronic diarrhea is a tough one. My first guess based on Dickson’s uncertainty (and Daniel’s statement that it would take some research) is cystoisosporoasis caused by C. belli. It is unusual but not unheard of for this protozoa to cause chronic diarrhea in immunocompetent patients. Infection comes from exposure to contaminated food or water. The patient’s family may well have had asymptomatic or mild symptoms which would explain why he reported them to be healthy.
Symptoms include:
- Profuse, watery, nonbloody, offensive-smelling diarrhea, which may contain mucus
- Foul-smelling flatus
- Cramping abdominal pain, vomiting (nausea and vomiting are uncommon)
- Malaise, anorexia, weight loss
- Low-grade fever
- Steatorrhea in protracted cases
- Myalgias (rare)
- Headache (rare)
Source: http://emedicine.medscape.com/article/219776-clinical#b3
Diagnosis can be confirmed with a stool examination for ova and parasites. This would be a good first choice since we are trying to minimize the number of unnecessary tests. This can rule out many other potential parasitic infections as well. If possible, a stool culture to look for usual enteric bacterial pathogens and fecal leukocyte exam would also be useful.
Treatment is usually TMP-SMZ (sulfamethoxazole and trimethoprim).
Differential is extensive. Cyclospora would be a good second likelihood and the lab should be notified to look for cyclospora of oocysts when performing the O&P. Dientameoeba fragilis usually does not present with steatorrhea and is negative radiologically. Giardiasis and cryptosporidiosis can be ruled out with a simple immunoassay, but we might want to wait since the symptoms would not be normal for either condition. Multiple bacterial infections are possible though these don’t usually last this long.
I look forward to the big reveal! I’m not as certain about this as I was about last episode’s unfortunate case, but either way I will enjoy finding out the answer!
Cool mornings and hot afternoons in the Eastern Sierra. School is now in full swing and we are hitting the tail end of the diarrhea season here in the clinical lab. We had our several cases of relapsing fever that we seem to get every summer, so our Borrelia species appear to be thriving in our tick population. No Lyme so far, to my knowledge, so probably hermsii or recurrentis. Soon we will be back to strep a and influenza before you know it.
Take care and keep up the great work!
Steve
Iosif writes:
Dear Twip Trio,
I don’t have a definite diagnosis for this case, but I’ll try to do my best.
My primary diagnosis is intestinal capillariasis caused by Capillaria philippinensis. They were discovered in the Philippines (hence their name), but are fairly prevalent in other parts of the world (such as Thailand). While birds are usually the definitive hosts for these nematodes sometimes humans can be used instead. The adult female worms can lay eggs within the GI tract that can either be excreted in the stool or mature within the tract and re-invade and re-infect the definitive host. This may explain why our fisherman is not getting any better. Symptoms include abdominal pain, weight loss, diarrhea, anemia and hypoalbuminemia. Steatorrhea is less common, but still occurs regularly enough that it doesn’t rule out the diagnosis.
Other secondary diagnosis:
Cholangiocarcinoma from chronic Opisthorchis viverrini/Clonorchis sinensis infection: Liver flukes are often asymptomatic themselves, but can become very symptomatic if a cancer sets in. Chronic infection with a liver fluke can irritate the bile ducts and eventually result in a cholangiocarcinoma. This could result in weight loss, fatigue and malaise. If the bile ducts were obstructed then a steatorrhea could develop with fat malabsorption; however, I doubt this diagnosis because the patient is not complaining of any RUQ pain. Jaundice, darkened urine, or light colored stools are also not mentioned.
A severe Ascaris infection could also obstruct the biliary tree via their huge mass. There would also be a significant anemia at that point from the significant amount of blood being lost by the parasites. Again this diagnosis is unlikely because there is no mention of respiratory complaints (although this is not always present) or an obstructive type of picture.
An Anisakis infection could also cause an obstruction if it formed a granuloma around the sphincter of Oddi. This is again unlikely from the lack of an obstructive picture (and possible pancreatitis that would result.)
For diagnosis a stool OVA and parasites would need to be done to look for eggs of these various parasites. For capillaria, I know that the stool OVA often come up negative and an EGD is done to look for the parasites directly, but I don’t know if this is available in the clinic within Thailand. Other exams that may help narrow the differential would be physical exam findings. How old is the patient (cholangiocarcinoma is less likely if he is in his 20s)? Is there any jaundice/pruritis? Any abdominal exam findings? Any eosinophilia (if available)?
Once again, thank you for a thought provoking case!
Sincerely,
Iosif Davidov
Hofstra SOM Class of 2018
Carol writes:
Greetings Team TWiP.
I’m writing from beautiful Vancouver Island, BC, where it is sunny and warm at 32C without a cloud in the sky.
My guess for the unfortunate boy in episode 114 is Naegleria fowleri, colloquially known as the brain-eating amoeba. The warm, fresh water made me initially suspect this, and the poor outcome reinforced it.
Caleb writes:
Greetings all:
Case Diagnosis:
I hope all is well and a new TwiP will be recorded soon. First off I would like to take a guess at the case presentation from TWiP 114. The 12-year-old boy brought to the hospital ER by parents with severe headache, stiff neck, fever, decreased alertness I believe has Naegleria fowleri or Naegleriasis. The severe headache, stiff neck, and fever are all classic symptoms of this infection. But what clinched the diagnosis for me, was that the boy was swimming in warm freshwater, a place where the amoeba can be found. The other very sad detail Dr. Griffin pointed out was the point that a pathologist was involved, and in a high percent of cases of Naegleriasis the patient does not make it. I want to thank you all for the time and effort you put into making these informative Podcasts.
Comments
On to a lighter note, first off I want to thank you again for providing such wonderful information from these podcasts, my wife (3rd-year medical student) just recently completed and did very well I might add on her Step 1 Boards. While studying for her exam she always dreaded studying the parasites, epidemiology, and drugs to treat said parasites, but with the help of this show I was able to sit down with her and we were able to go through parasite by parasite learning all about each one. While many of the parasites I had known previously to listening by TWiP, I am Ph.D. student in Medical Entomology, some of the parasites which are not transmitted via insect vectors, I did not know about. Through listening to this show I not only have passed countless hours in the lab running experiments but also found a practical application for the use of this newly acquired knowledge. So I thank you all very much.
Lastly, I have two fascinating (I found them fascinating, she, on the other hand, came home scratching, and disgusted) cases my wife has run into during her first few months of clinical training in the hospital. The first case was while she was working in the wound clinic ( She is currently at the V.A. hospital in Los Angeles) when a patient came in to have his soft cast replaced. As she was removing the soft cast, the patient began telling her and the resident that he was currently living with a friend who had Bed Bugs, and that he believed that the bed bugs had gotten into his cast and were biting him. As they continued to unwrap the cast, bed bugs began falling out of his cast and onto the floor. While she was telling me this story later that evening she was cringing at the fact that this patient had bed bugs, my only question to her was if she had collected any for me to look at.
The second case was again in the wound clinic when a patient came in who was non-ambulatory, and was brought in via wheelchair. As my wife and the resident approached this patient, the resident noticed that the patient had a layer of crust all over his hands, and began asking the patient about it. The patient said that it had been there for a year or so, and the resident just thought it might have been a fungal infection of some kind. My wife politely informed her resident after leaving the room, that the crusted layer on the patient’s hands looked like Norwegian scabies. As it turned out, the patient was Hepatitis C, and HIV positive, and indeed had a case of Norwegian scabies. While Norwegian scabies had been discussed in their parasitology/ infectious disease course in her first year, she happened to remember me showing her pictures of it after I had listened to TWiP 97: The seven-year itch.
I would like to thank you all again for all the hard work you put into putting out these amazing Podcasts and to keep up the good work! I look forward to hearing TWiP 115.
Cheers,
Caleb Hubbard
Entomology Outreach Coordinator
Ph.D. Student: Medical and Veterinary Entomology
University of California, Riverside
Jeff writes:
Dear Doctors Thank you so much for the podcasts, so informative and very current especially twie. Anywho I believe that poor child even though it is extremely rare and often misdiagnosed as meningitis was suffering from Naegleriasis. Unfortunately he was not diagnosed in time, otherwise a course of treatment would have been therapeutic hypothermia and miltefosine. Thanks for sharing your fountains of knowledge. It is hot on long island i don’t do weather forecasting jeff
Anthony writes:
http://rspb.royalsocietypublishing.org/content/283/1836/20161278
Ruben writes:
Dear Vincent, Dickson and Daniel,
I have a strong suspicion that the 12 year-old has a rare case of the deadly Naegleria fowleri. The symptoms line up pretty well: fresh water ponds, stiff neck, brain swelling, rapid onset, eosinopenia.
The only hesitation with that diagnosis is that Naegleria is extremely rare: only 130 cases of Naegleria have been reported with only three survivors!
I do hope that the case Daniel presented is actually about one of those lucky survivors, namely a 12 year old girl who was treated with rifampin, amphotericin, azithromycin, fluconazole, and dexamethasone. I hope that Daniel just relabeled her as a boy to make it more difficult to find, but I really do not know.
Recently, an antiparasitic drug miltefosine was used with a partial success (one out of two survivors). Miltefosine may also help with Balamuthia mandrillaris, another likely suspect in this case, but I would like to stick with the Naegleria diagnosis (more of a guess).
Thank you for making my all times favorite podcast.
Best regards,
Ruben
UCSD School of Pharmacy
Anthony writes:
Up until maybe 20 years ago there were distinct seasons here in Jersey City. It generally got cold late in December and stayed cold until March.
 My speculation is that the several month long layer of snow protected the leaf litter underneath where adult insects, larvae, and eggs overwintered. Now, there’s a cycle of thaws and freezes that kill off many of the insects. Cicada grubs in deep earth around tree roots will be protected. Mosquitoes on the walls of sewers will do very well. Down there they can remain blissfully unaware of the slings and arrows of climate change and just enjoy the good fortune of an early spring.
My speculation is that the several month long layer of snow protected the leaf litter underneath where adult insects, larvae, and eggs overwintered. Now, there’s a cycle of thaws and freezes that kill off many of the insects. Cicada grubs in deep earth around tree roots will be protected. Mosquitoes on the walls of sewers will do very well. Down there they can remain blissfully unaware of the slings and arrows of climate change and just enjoy the good fortune of an early spring.
Politicians dramatically send out aviators to attack the summer wetlands to combat mosquitoes. It won’t be as interesting on the evening news, but eradicating the mosquitoes in the residential sewers during the winter will probably be a lot more effective.
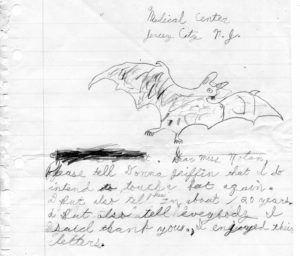
There are indeed bats in Jersey City. Around 50 years ago, I managed to rescue one knocked off the side of a house here in the Heights by water from a hose. Unfortunately, there was nothing like TWiV then, so I didn’t know anything about rabies. Neither penmanship nor artistic ability has improved.
Thank you.
Mo writes:
Hello TWIP friends –
Just wanted to drop you a quick line in response to the letter read near the end of TWIP #115 re: seemingly fewer insects to be found this year. I am somewhat relieved (yet also perplexed) to learn that I am not the only person who is seeing fewer insects this spring & summer, especially at night. I have always looked forward to finding many species of night-flying creatures at my porch light after sunset, but this year the offerings have been scarce to say the least.
I and others in my area have also reported a sharp decline in the number of Argiope aurantia (“writing spider”) this year as well. Most summers I can count between 15-20 mature females in my yard by August, but this year there are none! We do not use pesticides nor have we changed anything about our gardening, so it is a mystery to me where these beautiful spiders have gone.
The good news is that I have had an increase in the number of swallowtail and monarch caterpillars. In fact, I am on my way home now to check on a “ripe” monarch chrysalis to see if the butterfly eclosed today 🙂
The temperature in Norfolk, VA this afternoon is warm but pleasant at 84°F with 56 % humidity, a slight breeze and plentiful sunshine. I am enjoying my free trial to Curiosity Stream and intend to continue with a paid subscription when the trial is up – thanks for making this known and available to your audience. And thanks as always for all you do. Keep on twippin’ on.
Cheers,
Morgan
PS: I wrote to you earlier this year about entomophagy. It is probably safe to say that entomophagy is not popular enough yet to be the cause of the decreased number of insects many people have observed.
Sara writes:
Dear Twippers,
I am a new listener, having been directed to TWiP and TWiV by a fellow member of our medical school’s Infectious Disease Interest Group. I’m sad to admit our group only seems to have four members, but maybe that would improve if more of my classmates listened to your podcasts. I have yet to listen to many of the podcasts, but I have watched every episode of Monsters Inside Me, which emboldens me to venture a diagnosis.
My initial instinct, because you mentioned warm water exposure and an unfavorable outcome, is the tabloid-famed brain-eating amoeba, Naegleria fowleri, causing primary amebic meningioencephalitis. This would be consistent with the patient’s symptoms of headache, fever, stiff neck, and decreased alertness, as well as for the sad outcome of this case. Fatality rates for N. fowleri infection approach 99%. The majority of N. fowleri infections are in young males, like our patients, and it is not a geographically limited infection. (Acanthameba and Balamuthia could also cause an encephalitis, but generally only in immunocompromised patients, and with a less fulminant course.)
According to the CDC, imaging tends to be non-specific. Low glucose, high protein, and increased cellularity in the CSF are all consistent with N. fowleri infection. Bacterial meningitis would have some similar findings, but the patient did not improve with presumptive treatment and no bacteria were found in the CSF. I’m not sure what to make of the eosinopenia—but it can occur with protozoan infections, as I learned from episode 109, so perhaps that is the explanation.
N. fowleri could be diagnosed by visualizing the trophozoites in freshly acquired CSF, but unfortunately there is not an established treatment. Some have had success with amphotericin B plus rifampin, but there are too few known survivors of this infection to nail down the best treatment.
I’m not sure if my diagnosis is correct, but it’s my best guess. I’m excited to hear the answer and to have found your podcast.
Best wishes,
Sara
Trudy writes:
Dear TWiPpers,
Even though I’m a long time fascinated listener, I was not officially motivated to make a guess on your case studies until TWiP 114. Being a mother of two small children, the sudden death of the 12-year-old boy absolutely horrified me. Unfortunately, Dr. Griffin’s emphasis on the dog exposure and the mention of repeated mosquito bites threw me, so I never sent you my guess. However, now that I know the cause of the boy’s death, I feel compelled to write to you due to a couple of personal experiences.
Almost exactly a year ago, a friend of mine here in Atlanta, GA, was hospitalized with an inexplicable encephalitis, which three weeks later turned out to be fatal. Tragically, she left behind a husband and two little girls. To my knowledge, no autopsy was performed, and apparently the cause is still unknown, although West Nile virus and Naegleria fowleri were among the speculative guesses. I was afraid to ask her husband about it, as he was busy dealing with the aftermath of the situation.
I attached a couple of articles about this baffling case:
I also want to mention that I recently attended a company picnic at Fort Yargo Lake here in Georgia, where I took both my two-year-old daughter and six-month-old son into the water with me. I tend to live my life according to cost-benefit analyses based on factual information, rather than based on fear, and I simply wanted my daughter to have some unimpeded fun in the water. However, at that point I had not yet heard episode 115 of TWiP, and I must admit that I am now full of anxiety, especially considering the recollection that my daughter did stumble at some point, briefly submerging her head underwater. As I was listening to episode 115 on my drive in to work this morning, August 31st, I had to pull over and look up the incubation period for Naegleria fowleri, which according to various internet sources is anywhere between 1 to 15 days. Even though the skeptic in me tells me that we’re not 100% in the clear, I have to admit that I breathed a huge sigh of relief, as our little excursion took place on the 14th.
 I’m not sure if this means that we will never swim in lakes again, but I might limit our exposure to deeper areas of the lake, rather than the beach front. As I understand it, the amoebae live in the dirt, correct?
I’m not sure if this means that we will never swim in lakes again, but I might limit our exposure to deeper areas of the lake, rather than the beach front. As I understand it, the amoebae live in the dirt, correct?
Thank you so much for continuing to further my knowledge!
All the best from a shaken, but slightly empowered mom,
Trudy.
P.S. I attached a picture of my kids and me in the lake.

One comment on “TWiP 116 letters”