Håkon writes:
Greetings from sunny Athens GA,
Thankful for another brain stimulating parasitic question. Heard china and cysts and went to echinococcus multilocularis immediately given the prevalence. However, I couldn’t discount taenia coenurus. Figure either way treatment is surgical removal. Thanks,
Håkon
Stefan writes:
Dear TWIP-team,
hello again from Heidelberg, Germany, today it is 19°C and overcast but occasionally the warm sun is coming through, perfect weather for hikes around our castle ruins!
Excuse me for my lengthy reply for the challenging case in the last episode, today I will try to be more concise!
The man’s symptoms are consistent with equina/cauda syndrome, suggestive of lower spinal cord compression. The hints provided would suggest cystic echinococcosis caused by the dog tape worm Echinococcus granulosus to be the most likely parasitic cause, pending confirmation.
As a child the patient seems to have ingested eggs by food contaminated with dog feces (definite host), the human serves as dead-end host and typically develops cystic lesions (hydatid cysts) in the liver with protoscolices inside (in normal intermediate hosts like rodents these are eaten and develop into adult tape worms in dog intestines). If removed surgically without thorough precautions, these intermediate parasite stages may spill into the abdominal cavity or be carried away hematogeneously to other organs (typically lungs) and cause “metastatic” cystic lesions. Rarely, such as in this case bones may be infected. Here exophytic cysts (the one in the soft tissue of the buttocks?) can resemble hydatid cysts (endocyst, daughter cysts etc.), but in the bone this is not always the case as non-cystic tumorous growth in the bone leads to bone destruction. Diagnosis can be made serologically and by biopsy (PAS-positive membranes on pathology). Neurological symptoms may be alleviated by decompression surgery and other measures directed at stabilising the spine, but bone echinococcosis usually is not curable.
Life-long albendazole therapy may suppress further progression of the disease.
It would be interesting to learn under what circumstances the patientgrew up, whether the diagnosis was made at the time of the initial surgery and whether a spillage event was noted.
Stay save and all the best
Stefan
Rayna writes:
Hi there, thanks for the interesting cases! I’ve been newly introduced to the various TWis (Twix?) and have been really enjoying them. The May 1st episode was my first listen to TWiP.
The ddx from the listeners were quite involved and well thought out clinically! Veterinarian here, and a long time removed from clinical practise so here’s just a quick thought from the gut…for fun!
First twig was on the liver lesion and the early life dog exposure – made me think of cystic echinococcosis from E. granulosus, and although this can sit around latent for awhile, I didn’t think it really fit with the clinical picture. I think neurocysticercosis from Taenia solium fits better and Daniel answered my question about the patient, while being from a predominantly Muslim area, was not a practising Muslim, which makes it more likely in my mind that pork could be on the menu.
Anything on imaging that could confirm? High dose praziquantal and/or albendazole to treat for T. solium; if not, hydatid cysts are a lot more complicated to treat, I believe.
Thanks for the challenge!
Rayna
Dr. Rayna Gunvaldsen (she/elle)
Veterinary Program Officer, Import/Export Animal Products and By-Products
Canadian Food Inspection Agency, Government of Canada
Justin writes:
Hello TWIP presenters,
My name is Justin and this is my first time guessing for a case study, though I have been listening for several months now.
I recently finished an undergrad course in parasitology which I greatly enjoyed and now am going on to a master’s degree in parasitology after my undergrad in Biology at the University of Waterloo in Canada.
The weather here is mild and rainy at 9°C, the perfect weather for listening to the latest episode of This Week in Parasitism.
My guess for the parasite in this case study is Echinococcus granulosus causing cystic echinococcosis. The removal of a cyst from the patient’s liver as a child may have been incomplete and led to the seeding of a second-generation hydatid cyst in the buttock and spine. If indeed it was an E. granulosus infection, Albendazole and surgery were likely required.
Thank you for a wonderful podcast, and I look forward to listening to many more,
Justin
Jillian writes:
Good afternoon from a rainy 6C Ottawa, Ontario. Here’s hoping that all the rain means a lovely tulip season is about to bloom (we’re apparently home to the largest public display of tulips… who knew!).
Thank you as always for the interesting and engaging conversation and thank you to Eyal for the excellent cases in the previous episode.
Leaving aside the epidemiology for a moment, as soon as you start talking about progressive numbness, tingling (paresthesia), or weakness in the lower extremities – I immediately focused on lower spinal cord degradation or compression. The inclusion of a large palpable mass (hopefully it wasn’t palpated too aggressively!), in the buttock, would typically lead me to guess metastatic tumours, especially with loss of bowel control, but knowing that this is a parasitology podcast, coupled with the frequent mention of this individual’s exposure to dogs, lead me to ask if there are presentations of echinococcus granulosus involving the spine – which, indeed there are.
I’m not embarrassed to say that echinococcus infection has been one of my top 10 nightmare parasite infections since my parasitology prof first covered it (although our focus was on E. multilocularis due to our northern proximity), and this case certainly hasn’t changed that! For E. granulosus, transmission of this parasite occurs through a fecal contamination of the environment by canines (mostly dogs in rural areas) who act as the definitive host for the parasite. These themselves become infected by eating the offal of grazing animals (typically sheep) infected with the larval stages that hatch from eggs acquired from the environment. Humans however have a much worse time of things when they participate in the cycle, however unwillingly, as the larva, once ingested, can create fluid-filled cysts (hence hydatid – from Greek via Latin hudatis meaning watery vesicle) that can grow to rather spectacular size, resulting in organ damage if the cyst is within an organ (typically the liver), compression damage to surrounding organs, and also potential for anaphylactic shock if the cyst ruptures (say while an unsuspecting surgeon is trying to biopsy it).
In fact, although spinal hydatid disease is a relatively uncommon manifestation of infection with E. granulousis, it is relatively well documented in areas of high prevalence of the parasite, which include northwest China, particularly in the Xinjiang province (Yang et. Al, 2023). (The paper by Yang et al. is actually a trove of information about spinal hydatid disease in Northwest China and well worth the read IMO.)
Coming back to this specific case, Yang et al. also report that over 70% of individuals with spinal hydatid disease have a surgical history of hydatid infection, which likely speaks to the origin of the individual’s earlier liver cyst, as well as the large mass in the buttock. In cases like this, when the parasite invades the spine, there are no earlier clinical features, outside of those associated with spinal compression, as the cysts grows extremely slowly through bone, resulting in presentation 10-20 years following infection, which matches the individual’s reported dog exposure and the timeline for the first cyst being identified and removed. There is also the fact that Daniel was very reticent to share the findings of the CAT scan, which leads me to believe that it is relatively diagnostic, and although an MRI would provide better visualization of the spinal infiltration (Singh, et al., 2022), a CAT scan would likely show cystic bone destruction (Yang, et al. 2023), which along with the patient’s previous history of hydatidosis would be telling.
Definitive diagnosis would be by the aforementioned MRI and identification of cysts removed during surgery, perhaps PCR if you’re particularly curious of its lineage. Treatment would be cyst removal surgery paired with albendazole as an anti-infective treatment. In this case, although the individual had an earlier cyst removed, well even if the albendazole treatment was provided and followed appropriately, there is nothing to stop reinfection if the risk factors aren’t dealt with, which seems to be the case with prevalence of infection so high in this region.
Two quick questions for the experts if there’s time!
Even after all this time, I’m still not certain how to differentiate between cystic and alveolar hydatid disease in terms of presentation. I know that E. multilocularis infection is the more fatal of the two, and also infectious through those pristine-looking northern streams, but could you maybe expand on why? (again if there’s time!)
Regarding ChatGPT – based on the predictive text nature of the tool – I wonder if you’d find a difference in a medical answer based on how you identify patients… For instance, patient vs individual vs infected person… It could be interesting to see if that changes the type of intervention that ChatGPT suggests!
Thank you as always for such an interesting show!
Jillian (Learning Specialist)
Yang, L., Tuxunjiang, P., Liu, W. et al.Vertebral and pelvic echinococcosis in northwestern China. International Orthopaedics (SICOT) 47, 1153–1162 (2023). https://doi.org/10.1007/s00264-023-05731-y
Singh, N., Anand, T. & Singh, D.K. Imaging diagnosis and management of primary spinal hydatid disease: a case series. Egypt J Radiol Nucl Med 53, 106 (2022). https://doi.org/10.1186/s43055-022-00785-1
Pamir, M., Ozduman, K. & Elmaci, I. Spinal hydatid disease. Spinal Cord 40, 153–160 (2002). https://doi.org/10.1038/sj.sc.3101214
John writes:
Greetings Helminth Heroes,
I am writing from Cape Elizabeth, Maine, where the sun has finally returned after a brief deluge. Taking advantage of the balmy 65 degree F weather to mow the lawn while listening to TWIP, I thought it was high time to venture a guess at the case of the man from Western China with new cystic lesions in the bone.
Your clues of dog contact around the time of removal of a cystic liver lesion points me toward a diagnosis of hydatid disease due to echinococcosis. Echinococcus multilocularis seems the more likely species to “metastasize” to bone, but this may also occur rarely in E. granulosus hydatid disease if the cystic germinal layer from which the brood capsule arises is not carefully removed at the time of surgery. I think it is more likely that the initial infection was due to E. multilocularis, which may manifest as new lesions many years after initial presentation due to its slow growth. The CDC DPDx website states that E. multilocularis is endemic in China and is most commonly reported in Western and Northeastern regions where the parasite is present in wildlife populations.
I hope I have not embarrassed my teachers by being too far off the mark. I am taking the Global Health and Humanitarian Medicine course offered by Medecins Sans Frontieres, and had the pleasure of joining Christina’s parasitology lab training in Glasgow. I also enjoyed Daniel’s globe-trotting lecture “Cases Around the World” as part of the course.
As a septuagenarian who seeks opportunities to stimulate synaptic plasticity and neuronal connectivity, I am grateful to all of you for your scholarly and entertaining podcasts. Fingers crossed for next month’s DTMH exam.
Best,
John
First Vienna Parasitology Passion Club write:
Dear Hosts,
We are writing to you from very rainy Boston and sunny Vienna, since the two halves of our parasitology club live on separate continents. But we always have a great time working on TWIP cases together, despite time zone differences.
In this case, a thirty year old male patient presents in north-western China with right lower extremity weakness, numbness and problems regarding bowel and bladder function. He reports having had contact with dogs at a younger age and that he had a lesion removed from his liver in the past. He also has a mass in his right buttock, eosinophilia and CRP elevation. A CT scan shows cystic lesions and severe destruction of the lower vertebrae and coccyx.
When we heard this, it immediately made us think of cystic echinococcosis because we had recently seen a patient, who almost had the same clinical presentation as the patient from your case. The infection is caused by either echinococcus granulosus or echinococcus multilocularis, tapeworms which are mostly transmitted via the feces or urine of foxes and dogs.
After infection with the larvae, hydatid cysts grow in the liver, but can also be found in the lungs, the spine or in other parts of the body. Infection is oftentimes asymptomatic for a long time but when symptoms occur, they may include weight loss and pain in regions affected by the cysts. In this case, the patient’s symptoms most likely result from compression of nervous tissue in the vertebrae.
Diagnosis is usually made by ultrasound, MRI and CT scan and aided by serology, which can only confirm contact with the pathogen.
The treatment of echinococcosis is complicated and may involve the PAIR procedure (Puncture, Aspiration, Injection, Re-aspiration), complete surgical removal of the cysts and prolonged antiparasitic treatment with albendazol or mebendazol. As always, prevention is the best intervention, which is mainly achieved by washing one’s hands thoroughly, not eating fruit and vegetables collected directly from the ground and avoiding contact with wild foxes and unknown pets.
Thank you for this great case. All the best,
Michelle and Alexander from the First Vienna Parasitology Passion Club
Michael writes:
Hello,
I just ‘discovered’ your show last week and I enjoy it greatly. Thank you for putting together such interesting discussions and making them so entertaining!
Regarding the case of the week, given the history of ‘dog exposure’, liver lesion excision in the past, current bone and soft tissue lesions, and the fact that we are discussing parasites only (therefore excluding fungal and bacterial infections that could also present in similar fashion), my first diagnostic hypothesis is of echinococcosis. Other parasitic infections that could also present with bone and soft tissue lesions and that should be included in the differential would be toxoplasmosis, cysticercosis, toxocariasis, and sparganosis. Both Echinococcus granulosus and Echinococcus multilocularis are associated with dogs (i.e. their definitive host), can be found in Asia, and are known to cause liver, lung, soft tissue, and, occasionally, bone cysts. Toxoplasma can be seen both in cats and in dogs and can occasionally cause bone and soft tissue cysts (albeit bone cysts would be quite uncommon). Cysticercosis could present as bone and soft tissue cysts as well, but T. solium is associated with pigs and would be somewhat unlikely given the clinical history for this case. Toxocariasis is associated with dog exposure and it very rarely can be associated with spinal cord involvement, but it tends to present as solid masses instead of cystic lesions as seen on this case. Last, sparganosis (a rare infection caused by cestodes of the genera Spirometra and Sparganum) is associated with dog exposure, has worldwide distribution, and can cause both soft tissue and intraosseous lesions with associated weakness and numbness.
Concerning the next steps (and assuming only parasitic causes as this is TwiP ;-), I would order serological testing for Echinococcus by sequential combination ELISA and indirect hemagglutination methods followed by confirmation with immunoelectrophoresis and immunoblotting. If tests are negative, additional testing for other organisms could be pursued, including O&P, serologic testing for toxoplasmosis and toxocariasis, antisparganum IgG antibody, and immunoblot for T. solium assay. If tests are negative and the degree of suspicion for infection is still high, a FNA of the bone lesion with fluid analysis and/or a biopsy of the soft tissue lesion could also be pursued (this could be helpful for the diagnosis of Sparganosis).
Best regards,
Michael Waisberg, MD, PhD
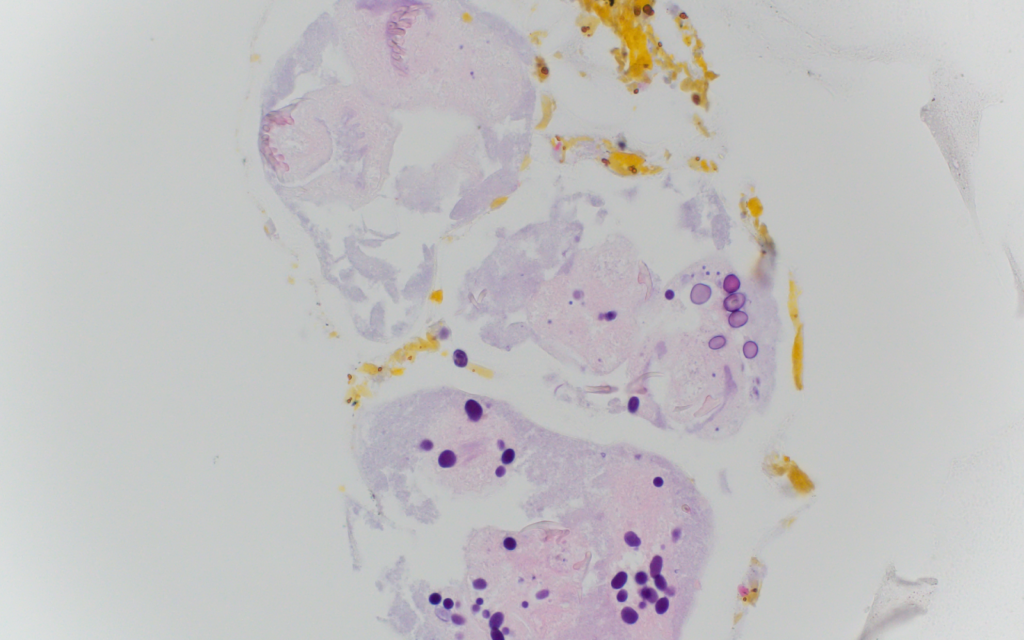
PS: Please find attached a couple pictures of a recent Echinococcus case I diagnosed by cytology.

Don writes:
My apologies if you’ve already received a dozen of these.
Kind regards and thank you all so much for your work. Your podcasts are the listening highlight of my week.
Don Norris, Sydney Australia
James writes:
I’m preparing a Clinical Integrative Session for our first year Medical Students on…parasitology! Just listened to your last case yesterday and learned some cool stuff about Malaria, Doxycycline, etc. As a pathologist I never prescribed Doxy for anything, much less Malaria.
This case of cystic lesion in young man in NW China of course smells like Echinococcus hydatid cyst disease with the dogs etc. Google tells me that Echinococcus is common in NW China associated with dogs and various herbivores. (I’ve seen a case in Utah in immigrant Basque shepherds though.) This is far and away my favored guess.
Differential Dx of cystic lesion causing neurologic symptoms…I’m guessing Cysticercosis from Taenia solium is not that likely but possible, especially if there are a bunch of similar sized cysts. Amebic abscesses? Does “sort of” tie up Liver and soft tissue cysts. Paragonimus lung fluke does make cysts but normally not gluteal cysts. Here’s a real stretch: squamous carcinoma from S. haematobium eating into the spine. Sometimes SCC looks cystic.
Thanks again for entertaining and educating me on my commute.
James M. Small, MD, PhD, FCAP
Professor of Pathology and Microbiology
Director of Clinical Career Advising
Rocky Vista University
Jason writes:
Greetings TWiP hosts!
It is a warm 32 degrees C here in Accra as I write this.
For the TWiP 216 case of the Hair of the Dog, I am going with a diagnosis of cystic echinococcosis. Our patient with a history of dog exposure at an early age appears to have had a hydatid cyst surgically removed from his liver some years ago. That removal seems to have been complicated by the accidental spillage of daughter cysts into the peritoneum which have evidently taken up residence as hydatid cysts in their own right. This secondary hydatidosis might have been prevented with an intraoperative peritoneal lavage of a scolicidal agent such as hypertonic saline, and prophylactic administration of albendazole.
Worm regards,
Jason
Marcus writes:
Dear TWiP-team, you are still Best in Show, keep hounding us with these great cases.
Here it stopped snowing a week ago, and now we have a lovely sunny day with a warm 14C in central Norway.
Sorry about the following digressions, feel free to skip the first few paragraphs of differentials, and go straight to the case guess.
So my guess initially came to me when Daniel mentioned dogs and the removal of unspecified objects from livers. The attempts at back pedaling regarding the dog were not particularly effective, and didn’t end up changing my answer.
Differential and clinical reasoning:
Before we get there though, I think we should look at some of the ideas that didn’t quite make it. I once learned that when making a diagnosis, you should always come up with at least three well thought out differentials; with at least two horses, and one zebra. Though the zebra may almost never be the right diagnosis, the exercise does keep you on your toes when one does show up in your emergency room.
First – the common, non-parasitic alternatives. If we had no CT-scan upon presentation, a lumbar prolapse with cauda equina syndrome is by far the most likely, followed by traumatic injury to, or compression of the medulla, or medullary infarction. Metastases seem unlikely, considering his age. Since he has some raised inflammatory markers, it is worth considering infectious causes, such as discitis or osteomyelitis, and always keeping TBC and syphilis in mind, as well as other inflammatory illnesses like a strange presentation of Guillain-Barré syndrome/AIDP or transverse myelitis.
A more thorough neurological exam distinguishing between upper and lower motor neurone symptoms should be conducted.
Now, moving on to the possible parasitic causes. Cysticercosis! Medullary cysticercosis has been reported, as well as medullary compression from extramedullary cysticercosis. Daniel made a point of the patient not being a muslim, in a predominantly muslim area; which may be relevant. Interestingly, in muslim countries with the Kafala system, it is in fact often the masters who eat halal who get cysticercosis, while their servants/slaves (who eat pork) do not. The servants have regular pork tapeworm disease; this being because they are infected by cysts from eating pork, that will develop into regular tapeworms in the gut. The masters, on the other hand, are infected directly by eggs from human faeces, without going through the porcine stage, allowing for tissue migration, including migration to the CNS. Does not fit with the CT-scan though.
Katayama fever again can cause cauda equina-like symptoms, though I would not give this finding on CT. Furthermore, the CNS-symptoms of schistosomiasis are usually only evident upon initial infection in naive travelers, not in people living in endemic areas. Furthermore, Daniel denied any nearby sources of fresh water.
Case guess:
So I return to my first thought – Medullary compression from hydatid disease of the bone, caused by echinococcus granulosus (the dog tapeworm). Regular hydatid disease is a cystic disease, usually presenting with liver cysts containing scolices. Previously treated by surgical removal of the whole cyst (puncturing it may cause a massive immune response, anaphylaxis and death), PAIR-procedure is currently preferred in most setting. Though rarely metastatic, the most common location for bone spread is the spine and sacrum.
Assuming a hydatid cyst was removed from our patient, If any small cysts and scoleces were left after surgery, and metastasized to bone, their growth would be slow. Decades may pass before any symptoms present, typically back pain, pathological fractures, and focal neurologic deficits.
The CT results are also consistent with this diagnosis. Serology with titres may be helpful if further confirmation is required. Removal of the cysts may be risky, because of the anaphylaxis risk. Treatment should combine removal of affected bone with some margin, PAIR where possible, and systemic antihelminthics (albendazole). Since it is unlikely all microcysts will be removed in widespread disease, any treatment could be considered palliative.
Keep up the great work, hope to see you all in Chicago!
Marcus
PS. I use the word metastasis intentionally here, as I think it describes the spread of hydatid disease well. It does, however, describe it´s sister E. multilocularis (the fox tapeworm) even better, which even looks like a malignancy on imaging.
PPS. Concerning primaquine and G6PD-deficiency, we might have to reconsider our understanding a bit. In general, the G6PD-problems with various medications may be a bit overstated, recently pointed out in Taylor et al 2023 in the Lancet – Infectious disease.
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(22)00658-2/fulltext
Kimona writes:
Dear TWiP Team,
A great thank you for inspiring Maureen and I to share a properly splendid weekend together in NYC, surrounding your TWiV 1000 event. So nice to see and hear you all in person!
As for this month’s case – I learn the most when I am forced to go down multiple ‘rabbit-holes’ during my researching and am therefore staying away from the “AI” query thing….for now (or until my teenage kids show me how!)
I am postulating that the 30 y/o male with weakness, bowel/bladder dysfunction and a remote history of liver lesions, has a persistent and secondary spinal Echinococcus granulosus infection.
E. granulosus is one of the smallest cestodes, a tapeworm that lives within the small intestine of the canine family, shedding embryonated eggs into the feces, and thus afflicting any herbivorous animal or human that encounters such contaminated soil/plants. These infections are endemic in any area where sheep husbandry and their dogs are prevalent, including NW China. Once eaten, the oncosphere hatches in the small intestine of humans and enters the bloodstream, reaching the liver via the portal circulation. It can invade most organs, although over 90% of cysts are found in the liver or lungs. Larvae synthesize a surrounding hyaline membrane which differentiates into an outer, acellular structure and an inner cellular germinal layer, which gives rise to protoscolices. Any spillage or rupture of cyst fluid can lead to secondary spread, since these germinal layer cells have a stem cell-like ability to reproduce a full hydatid cysts, causing disease of newly invaded tissues, as in this man’s spinal Echinococcosis. These cysts grow at a slow rate of 1-5cm/yr and would account for his very delayed presentation, now almost 25 yrs after first exposure as a child.
Hydatid disease in the spine presents similarly to this man’s – at a rather late stage and with symptoms of pain, swelling, pathologic fracture of bone, and/or neurological compromise, such as weakness and bowel/bladder dysfunction if there is sacral nerve involvement.
It is plausible that there was either leakage or incomplete excision of all daughter cysts during his childhood liver lesion removal. Perhaps the mass felt in his right buttox is due to an expanding lumbo-sacral bony lesion? The elevated ESR and CRP, generally non-specific markers of inflammation, could be response to a localized infection of the bone, such as osteomyelitis or a walled off bone abscess. His normal white blood cell count may be due to the parasite’s known production of immunosuppressive substances. Only after release of a cyst’s antigenic fluid and protoscolices, is there risk of a host’s anaphylaxis response.
For diagnosis, imaging using ultrasound, CT and MRI, can be helpful in detecting cystic lesions. On X-ray you may see calcified cysts in tissues or destructive lesions in bone – the latter which can easily be misdiagnosed as tuberculosis, bone cysts, and metastatic disease. Serological tests include ELISA to detect plasma antibodies to Echinococcus, and further detection of different Echinococcus antigens by immunoblot assays. Microscopic identification of hooklets from an aspirate (or sputum from lungs) can also be diagnostic.
Treatment comprises mainly a combination of surgical and chemotherapeutics. The PAIR technique of puncture, aspiration, injection, and re-aspiration using ultrasound guidance has replaced surgery for some patients with liver or other solid organ involvement. However, spiny/bony Echinococcus poses challenges due to the difficulty in complete excision of these lesions and surgery often takes on a more palliative role. Combination therapy is used with Albendazole and Praziquantel, both pre- and post-operatively for varying lengths of time. I read that Praziquantel is mainly useful in early disease and less for treatment of mature cysts and that most scolecidal agents don’t eradicate all daughter cysts. This likely explains the rather unimpressive resolution rates and significant relapse rates.
In the interest of this young man’s prospects, I am hopeful that my diagnosis is either wrong or that there are newer treatments with improved eradication rates of Echinococcus of the spine.
In anticipation of the reveal! And warm regards from a now gorgeously sunny Vermont!
Kimona
Chris writes:
Good morning hydadid twips,
I was on a post-Internal medicine-shelf exam road-trip listening to old episodes of TWIP when Dr. Despommier made an interesting comparison between Hydadid Cysts disease, caused by the dog tapeworm, and cancer in TWIP #7. It’s an apt comparison! If the cyst of Echinoccous granulosos ruptures, two big problems can occur. Problem one relates to our body freaking out and producing a life threatening anaphylactic reaction to the parasitic antigens. Problem two is far more interesting. Within the larger hydadid cyst float many daughter cysts that, if leak out into the body, can spread in a similar fashion to a metastasizing tumor. If the daughter cysts find themselves in a critical area, such as next to the sacral nerves, they can grow and physically damage or compress the surrounding structures, causing significant signs and symptoms. Tumors, depending on sarcoma or carcinoma, tend to spread via blood or lymph. Do hydadid daughter cysts spread similarly or do they implant wherever they land? Additionally, does Echinococcus Multilocularis, the fox tapeworm responsible for alveolar echinoccocus, grow daughter cysts in humans as well or do the stem cells themselves have the potential to spread around the body?
I think this is what’s going on with our patient. He had a hydadid cyst removed many years ago but many daughter cysts unfortunately leaked into his body during the procedure. Over the years, they have grown, causing what sounds a lot like cauda equina syndrome or at least damage to important sensory and autonomic function nerves, leading to his presentation. Draining the existing cysts must be done with great care to prevent further spread of daughter cysts, with some recommendations suggesting treating with the PAIR procedure: puncture, aspiration, injection, and reaspiration with a scolicidal agent such as 95% ethanol. Some suggest adding albendazole to the treatment regimen.
Thank you!
—
Christopher Hernandez
David Geffen School of Medicine at UCLA, Medical Student
MPH, Infectious Diseases and Vaccinology
University of California, Berkeley
Mark writes:
Dear TWiPers,
I write to submit my diagnosis for episode 216. ChatGPT was not used in this analysis.
I believe the 30 year old man in rural China is suffering from Toxocariasis from exposure to T. Canis eggs. According to the CDC, treatment is 400 mg of Albendazole taken orally twice a day for five days.
The key to my diagnosis was mention of “dog exposure” in the case notes: “When he was just a few years old he had reported dog exposure and had a lesion removed from his liver”
A Google search for “dogs humans zoonotic parasites” identified hook worms and round worms as possible causes. Hookworms are eliminated because their signs & symtoms don’t match the case description.
Roundworms, aka Toxocara canis, infect humans via swallowing eggs from dog feces. Young children playing with dogs and swallowing feces-borne eggs is a common vector. (References: “Infectious Disease 7th ed”, or this review article written by Dickson in PubMed https://www.ncbi.nlm.nih.gov/pmc/articles/PMC153144/).
Worms can travel throughout the body, and many sufferers are asymptomatic. I speculate that this patient was treated for Toxocariasis by removing the lesion in his liver. It appears this did not completely eliminate the infection – there could have been latent worms elsewhere in his body — or perhaps he got reinfected. The worm can live within muscle or bone which match the case description – the mass in the buttock and destruction of bones in the cited locations.
Local surgery can’t compete with system-wide use of Albendazole. Is this a good case study for treating symptoms and not curing the underlying disease?
ELIZA tests are available for diagnosis of Toxocariasis. No mentions were made of these. Maybe they were not available in that region of China? Instead the case notes indicate “ESR and CRP are elevated”. These are tests for inflammation and their “elevated” levels are consistent with his body’s increased immune response against an infection, likely the Toxocara worms.
Moving on … it was great meeting Daniel, Dickson, and Vincent at the TWiV 1000 celebration event. These case studies are very educational and transform TWiP into an active learning experience. Have you considered adding case studies to other shows? Here is an idea for a new Microbe.tv show “Name that Pathogen” – make a short show entirely about presenting a case study signs & symptoms and panelist recommendations for needed diagnostic tests, identification of the disease and indicated remedies.
Mark
Paul writes:
Dear TWIP World Citizens,
Many thanks to all of you for your fine work. Avid TWIV listener, newly listening to TWIP.
Writing from Petoskey, Michigan on the shores of Lake Michigan’s Little Traverse Bay, cloudy and 47 F with rain earlier.
Quote: “Medicine is a science of uncertainty and an art of probability” – Dr. William Osler
30-year-old man from Xinjiang China with right leg numbness and weakness, bowel and bladder dysfunction and right buttock lesion with cystic structure invading spine and sacrum and history of dog exposure and liver lesion removal in childhood. Lab evaluation: normal white blood cell count, elevated inflammatory markers, negative HIV testing.
Differential diagnosis:
1. Cystic echinococcus infection due to Echinococcus granulosis.
Other considerations since the clue “this is a podcast about parasites” isn’t always available:
2. Malignant sarcoma invading bone.
3. Malignant osteosarcoma
4. Tuberculosis of the lumbar spine and sacrum with cold abscess.
5. Plasmacytoma due to multiple myeloma: very unlikely, patient too young.
Epidemiologically cystic echinococcus fits very well as there are abundant sheep in Xinjiang combined with the history of dog exposure. The clinical course of a slowly evolving cystic disease over decades also fits.
Next steps: Serologic testing for Echinococcus.
If confirmed, treatment: Albendazole for a number of months. Injection of the cyst with protoscolicidal chemical solutions followed by surgery may be important in this case to forestall further neurological deficits. Caution that leaking cyst contents can precipitate anaphylactic shock.
Paul Blanchard, MD
Older general internal medicine physician with no parasitic disease experience.
Martha writes:
Dear TWiPers
I hope I’m not too late again. I tend to get side tracked when I start browsing for your cases. The region of Urumchi was mentioned, which reminded me of the interesting book by Elizabeth Wayland Barber, the Mummies of Urumchi. I went looking for the book and I have come to the conclusion that I’ve loaned it to someone and never had it returned.
This has nothing to do with the case of the young man with weakness in the right lower extremity and pelvic floor issues. He has a palpable mass on the right upper buttock and CT shows a mass encroaching on the spine at L5 and below. We are told he had exposure to dogs in very early childhood; the exposure is unspecified and the type of dog is not mentioned. He seems to have been too young to be out managing a flock with the aid of sheepdogs. We are also told he had a liver lesion removed in childhood. I wonder if the pathology report is available.
The parasite that I suspect is Echinococcus granulosus. This tapeworm’s life cycle has the dog as the definitive host and the sheep as intermediate host. The dog becomes infected by being fed offal containing the E. granulosus cyst from slaughtered sheep. Sheep become infected by ingesting the embryonated eggs shed in the dogs feces.
For definitive diagnosis a fine needle aspirate could be done and rule out other causes such as TB or malignancy. I am led to believe that antihelminthic agents followed by surgery is the consensus for treatment.
I hope this finds you all well and that I have not again delayed too long in responding
Best wishes to all
Martha
Felix writes:
Dear Twip Team
my last two guesses were sent in too late so I hope this one finally makes it. When I went climbing in China, I learned the valuable lesson to always check the rented gear! We went on a two day trip and when we arrived at our camping spot and tried building up the tent, we realized that the rain cover was missing. Well when I started raining in the evening laying in the water was way too cold so we just climbed through the rainy night and at least we were rewarded with being the only ones at the summit by sunrise.
Now to the case.
My guess for this patient is ecchinococcus granulosum, especially with this history. If this wouldn’t be a parasitology podcast, malignant causes would be on the differential list too.
So what to do now? First some bloodwork could be done looking for the elevation of antibodies. I think they have a certain threshold for acute disease. If my guess is right, drainage or biopsy is probably too risky. Since there is acute worsening neurological presentation, spinal decompression and cyst excision should be done if the patient is healthy enough for operation.
I really like the chatGPT emails, it’s stunning what a non-medical-meant transformer network can produce!
Greetings from Germany
Felix
Inge writes:
Dear professors at TWiP
How grateful I was when I discovered your podcast about this topic that has had my passion for quite a while. I am a young doctor from the Netherlands but with an ever growing interest in tropical medicine since having lived in Mozambique for several years as a child. I hope to be able to work in Africa myself one day, when the time – and my education and experience – is ripe. Since my high school thesis about malaria, I have had a particular love for parasites. I feel like they always carry a story with them, their life cycle can explain so much about symptomatology and somehow personifies them. While travelling in Africa in between jobs I had more time on my hands and wanted to get back into the hobby of studying parasites. You can understand my great joy when I found TWiP, with you being equally or even more passionate and talking about all these fascinating diseases with such insight. I can say I binged quite a couple of episodes before your latest one came out and I decided I would take my turn and give answering the case an actual try. Thank you also for mentioning the wonderful resource in Parasitic Diseases 7th edition.
Now, on to the case, a 30-year old male from China, with complaints of numbness and weakness in the right lower leg and a cystic lesion with significant destruction of L5 continuing into the sacrum and coccyx.
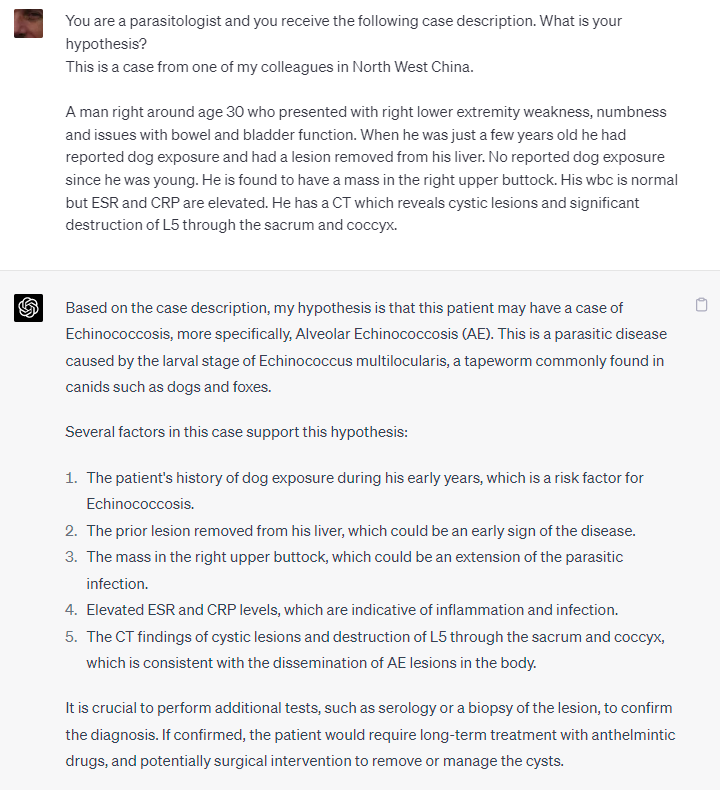
Being inspired by the previous case and its entries, I thought I would start out by giving Chat GPT a try, but merely for inspiration, as we have seen its limitations as well. I specified China as the location of occurrence, as your wonderful guest of last episode highlighted the importance of epidemiology in reaching a differential diagnosis. Chat GPT seemed quite convinced that the parasite we should be looking for is a tapeworm or cestode. Particularly high on its list was neurocysticercosis. With a little encouragement, it also named echinococcus, spirometra, and as non-cestodes, toxoplasmosis and gnathostomiasis. Looking into the case and diseases myself, I came to the conclusion that the tapeworms mentioned would be a very likely cause of the complaints. Ingestion of an embryonated egg of the tapeworm can lead to disease caused by the larvae lodging in tissues and creating space-occupying cysts. Taenia solium is known to cause neurocysticercosis, and echinococcus to cause hydatid disease. In comparison to Chat GPT I am leaning more towards echinococcosis as a cause. If I had to specify further, I would even bring up echinococcus multilocaris, but I am not confident enough to distinguish between the two types. Multilocaris would fit with dog exposure at a younger age and a presentation of disease at late adolescent to early adult age. With little to no experience in this field I will not say my feeling is very well informed, but my feeling leads me to think that neurocysticercosis would be more likely to occur higher up the central nervous system, and with the amount of destruction, the typical size of the cyst, which Parasitic Diseases mentions to be around 10mm3, I feel like neurocysticercosis is not as good a fit for the case description as echinococcus seems to be. I am not confident enough to distinguish between the two types of echinococcus, so I will leave it at that. My guess is that the complaints of this Chinese man are caused by the parasite echinococcus.
What I would like to do is to confirm this diagnosis using ELISA with the hydatid fluid antigen. A negative result is not enough to rule out the disease. People who have never had a cyst rupture may not have had enough antigens in their system to have created an adequate antibody immune response. The definitive diagnosis could be made using microscopic analysis of for example sputum. Finding hooklets in the sample would confirm the diagnosis. Noteworthy is the strict contra-indication to taking a biopsy of the cyst. This is particularly noteworthy because the finding of a destructive lesion in the spinal cord or surrounding bones would give good reason to suspect malignant disease as a cause, for which a biopsy would be the most important strategy to confirming the diagnosis.
The treatment consists of a combination of medical and surgical intervention, surgical being the removal of the hydatid cyst and possibly repair of the vertebral column by for example stabilization. Medical intervention would be treatment with antihelminthic drugs, for example albendazole 400mg BID for 1 up to 6 months.
Although I hope that my guess of echinococcus is correct, I look most forward to learning from all of the reactions of the other participants and what you will have to say about it yourself. I absolutely love what you’re doing, keep up this great informative work!
Greetings from a sunny day in Malawi, where rainy season is finally over and we’re moving into winter, with temperatures around 26 degrees Celsius. I will be enjoying the last days of our stay in my beloved Africa, kind regards to you all!
Inge
Leon writes:
Dear TWIP team,
The Chinese patient, who had a liver lesion removed during childhood and presents with a mass in the buttock and cystic lesions in the bones likely suffers from an infection with Echinococcus granulosus. Infection with this tapeworm is typically acquired through contact with infected dogs and remains asymptomatic for years. Epidemiological studies have actually shown that the highest risk of infection occurs during childhood which would fit together with the patients history of early contact with dogs. The ingested embryonated eggs hatch and develop into oncospheres, which predominantly migrate to the liver or lungs but can also affect other organs such as bones, the brain, and muscle tissue, forming hydatid cysts that can grow to a size of 5 – 10cm.
The patient’s right lower extremity weakness and numbness are likely caused by the destructive effects of the cysts on the lumbosacral joint, specifically affecting the L5 spinal nerve, which is essential for leg movements. The cysts affecting the spinal cord could contribute to the issues with bowel and bladder function, although they could also be caused by cysts in the respective organs. The detected elevation in inflammatory markers may be a result of the inflammatory processes occurring in destructed bone or other affected regions. The cysts themselves, unless they rupture, do not trigger a significant immune response due to immune evasion of the hydatid cysts, which explains the normal white blood cell count. The description of the mass in the buttock fits also together with the potential size that the cysts can reach.
To confirm the diagnosis, additional tests such as ELISA can be performed, although imaging techniques including ultrasonography, CT, and MRI remain the preferred diagnostic tools.
In the case of the patient proper imaging should find all cysts and the choice of treatment then decided based on the stage and location of the cysts. Minimally invasive procedures like the PAIR (Puncture, Aspiration, Injection, Re-aspiration) technique are often preferred for draining and treating the hydatid cysts. In some cases, surgical intervention may be necessary. Adjunctive therapy with albendazole is typically prescribed as well. Whether there can be anything done to recover motoric functions of his leg I don’t know but I hope so for the patient.
I hope this time I am correct with my diagnosis. I have also considered infection with the pork tapeworm, Taenia solium, but the patients history and symptoms fit better to Echinococcus granulosus.
I hope the patient is doing better meanwhile.
All the best from Germany,
Leon
Eyal writes:
Dear sages of microscopic eukaryote life.
Greetings from Sydney in the land down under.
The season of short days and long nights is almost upon us, and Covid is making the rounds again.
I’m currently isolating with a mild case of Covid, which anecdotally is much milder than the previous time around (14 months ago). I wonder about the breadth of my immune response after receiving the main series, a booster, then ‘BOOSTED’ with the original Omicron and now boosted again with one of the XBBs.
On to the case:
I found this one more challenging than normal. Especially based on the lack of guiding details. The only clues I could tease out are: North West China, dog (K9?), and some penetration into the spine (bone?) or the CNS. Also, I think there is a clear immune response based on the elevated ESR and CRP.
Based on the lack of clues I decided to take the epidemiological route:
Initially, I thought of a nematode infection that got into the CNS somehow. However, I couldn’t find any compelling literature.
So I finally landed on infection with, Echinococcus granulosus, which is a tapeworm endemic to the area which sometimes can infect the bones and is consistent with the Dog clue (lead :)) as the Dog is the definitive host.
My guess in terms of the next steps is PCR/blood test, probably a stool exam, not sure about the next steps as it seems that if the cyst ruptures it could cause an anaphylaxis shock and also lead to some sterilisation of the host?!? would love to understand more about this mechanism.
I apologise for the disorganised email (more than usual). Being hazy/foggy is still a symptom 🙂
Many thanks as always for everything that you do.
Eyal
Stacy writes:
I am so excited to be back listening to TWIP. Thank you for all that you do.
A Google search about the case of a 30-year-old with a mass in the right upper buttock, right-lower extremity weakness, numbness and both bowel and bladder issues took me directly to Hydatidosis, a disease caused by the larval form of Echinococcus granulosus. I found several articles referring to patients with cysts in their gluteal muscles, all of whom were treated with antihelminithic drugs, such as mebendazole and albendazole. But it was the article: Prevalence and Molecular Characterization of Echinococcus granulosus that made me decide to look no further. It says that sheep and cattle are a reservoir for E. granulosus, which means the young man did not need to be in contact with dogs to be infected. Also, E. granulosus is prevalent in the Xinjiang Uygur Autonomous Region – which is in the northwest of China, and whose capitol, Ürümqi, is 100 km west of Tianshan Tianchi National Park. I am guessing that Daniel mentioned this to help with location. (I used Wikipedia for geography).
The excellent article “A Solitary Abscessed Hydatid Cyst of the Buttock: A Rare Case” gives a wonderful summary of E. granulosus:
“The dog is the definitive host, and human infection occurs accidentally by ingestion of food contaminated with the parasite’s eggs or by direct contact with a sick dog. The ingested parasite eggs penetrate the intestinal wall and use the portal system to spread throughout the body. This explains the frequency of liver involvement (60%-70% of cases) … Unusual localizations have been reported, including bone (1%-3%) … joints, subcutaneous soft tissues, and muscles. The majority of reported cases of subcutaneous hydatid cysts are located in the thigh (27%), hypogastric region, thorax, and head and neck region. Gluteal localization is extremely rare (9% of subcutaneous hydatidosis cases).”
The elevated ESR and CRP tests and the CT scan showing cystic lesions is consistent with the diagnostic tests used in the articles I found on E. granulosus. I do not know what can be done about the young man’s spinal cord injury, which I am assuming is why he is now having extremity weakness, numbness and bowel and bladder issues. But giving him either mebendazole or albendazole and removing all cysts seems like a good start.
If I ever win a book, I will give it directly to my daughter who plans on heading to nursing school as soon as she completes her prerequisites. Before she goes, I figure I can peek at it as well.
Looking forward to hearing the solution, and how the young man is faring.
I love your podcasts!
Stacy
Stacy writes:
Hi Vincent, Dickson, Daniel and Christina,
Today, I decided to finally test ChatGPT. I first did a series of questions about UTIs, then switched to E. granulosus. This conversation is interesting to me because when I asked if E. granulosus caused damage to the lumbar vertebrae, it gave me two names for the condition: “vertebral hydatid disease or vertebral echinococcosis.” I looked up the first, and sure enough, I found the following article:
I had only two semesters of nursing school, which ended back in 2008, so I am not able to detect incorrect information given by ChatGPT, but I can do further searches using its terminology. This is where I think ai might really be useful. I was lucky when I did my Google search yesterday. Had I used ChatGPT after I discovered E. granulosus, I think my search would have taken less time.
I’m sending you the conversation, since it is an example of how a lay person like myself would use ai to look up medical information.
Thank you, as always, for this amazing podcast,
Stacy
Daniel writes:
Hello Twip team
My name is Daniel
My guess is the 30 year old male has Hydatid disease.
I believe the cystic lesions in his spine, soft tissue and previously in his liver are hydatid cysts acquired be ingestion of Echinococcus granulosus or Echinococcus multilocularis eggs in dog feces.
Thank you for the fascinating case studies.
I am currently reading your book “People, Parasites and Plowshares”, Dickson. I am on the chapter on Tapeworms which may have swayed my guess. I am thoroughly enjoying it.
Take care
Daniel
